Products & Services
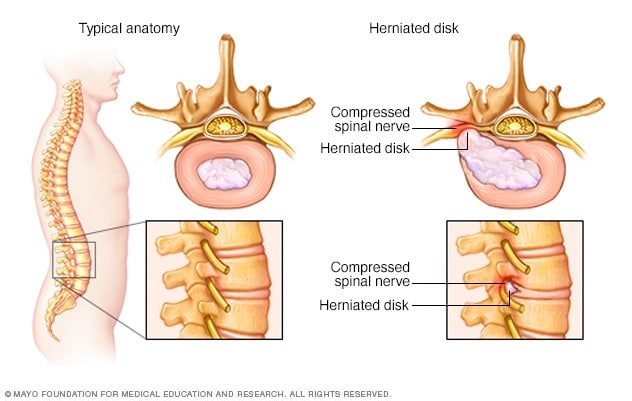
Most herniated disks occur in the lower back, although they can also occur in the neck. Signs and symptoms depend on where the disk is situated and whether the disk is pressing on a nerve. They usually affect one side of the body.
- Arm or leg pain. If your herniated disk is in your lower back, you'll typically feel the most pain in your buttocks, thigh and calf. You might have pain in part of the foot, as well. If your herniated disk is in your neck, you'll typically feel the most pain in your shoulder and arm. This pain might shoot into your arm or leg when you cough, sneeze or move into certain positions. Pain is often described as sharp or burning.
- Numbness or tingling. People who have a herniated disk often have radiating numbness or tingling in the body part served by the affected nerves.
- Weakness. Muscles served by the affected nerves tend to weaken. This can cause to stumble, or affect your ability to lift or hold items.
Factors that can increase your risk of a herniated disk include:
- Weight. Excess body weight causes extra stress on the disks in your lower back.
- Occupation. People with physically demanding jobs have a greater risk of back problems. Repetitive lifting, pulling, pushing, bending sideways and twisting also can increase your risk of a herniated disk.
- Genetics. Some people inherit a predisposition to developing a herniated disk.
- Smoking. It's thought that smoking lessens the oxygen supply to the disk, causing it to break down more quickly.
Seek emergency medical attention if you have:
- Worsening symptoms. Pain, numbness or weakness can increase to the point that they hamper your daily activities.
- Bladder or bowel dysfunction. Cauda equina syndrome can cause incontinence or difficulty urinating even with a full bladder.
- Saddle anesthesia. This progressive loss of sensation affects the areas that would touch a saddle — the inner thighs, back of legs and the area around the rectum.
To help prevent a herniated disk, do the following:
- Exercise. Strengthening the trunk muscles stabilizes and supports the spine.
- Maintain good posture. This reduces pressure on your spine and disks. Keep your back straight and aligned, particularly when sitting for long periods. Lift heavy objects properly, making your legs — not your back — do most of the work.
- Maintain a healthy weight. Excess weight puts more pressure on the spine and disks, making them more susceptible to herniation.
- Quit smoking. Avoid the use of any tobacco products.

Physical therapy often plays a major role in herniated disc recovery. Involving below key points
- Ambulation and resumption of exercise
- Pain control
- Education re maintaining healthy weight
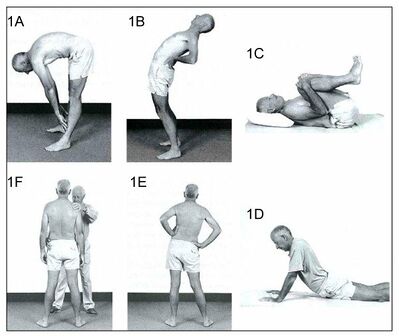
There are a number of exercise programmes for the treatment of symptomatic disc herniation eg
- aerobic activity (eg, walking, cycling)
- directional preference (McKenzie approach)
- flexibility exercises (eg, yoga and stretching)
- proprioception/coordination/balance (medicine ball and wobble/tilt board),
- strengthening exercises.
- motor control exercises MCEs
They are a common type of therapeutic exercise prescribed for patients with symptomatic disc herniation.
- designed to re-educate the co-activation pattern of abdominals, paraspinals, gluteals, pelvic floor musculature and diaphragm
- The biological rationale for MCEs is primarily based on the idea that the stability and control of the spine are altered in patients with LBP.
- programme begins with recognition of the natural position of the spine (mid-range between lumbar flexion and extension range of motion), considered to be the position of balance and power for improving performance in various sports
- Initial low-level sustained isometric contraction of trunk-stabilizing musculature and their progressive integration into functional tasks is the requirement of MCEs
- MCE is usually delivered in 1:1 supervised treatment sessions and sometimes includes palpation, ultrasound imaging and/or the use of pressure biofeedback units to provide feedback on the activation of trunk musculature
- A core stability program decreases pain level, improves functional status, increases health-related quality of life and static endurance of trunk muscles in lumbar disc herniation patients. Individual high-quality trials found moderate evidence that stabilization exercises are more effective than no treatment.
- Different studies have shown that a combination of different techniques will form the optimal treatment for a herniated disc. Exercise and ergonomic programs should be considered as very important components of this combined therapy.
General rules for exercise/ Do and Donts
- Do exercise slowly. Hold exercise position for slow count of 5. Start with 5 repetition and work upto 10. Relax completely between the repetitions.
- Do exercise for 10 min twice a day.
- Care should be taken while doing exercise which can be painful.
- Exercise daily without fail.
Physiotherapy Modalities and the evidence for their use in disc herniation
- Stretching - There is low-quality evidence found to suggest that adding hyperextension to an intensive exercise programme might not be more effective than intensive exercise alone for functional status or pain outcomes. There were also no clinically relevant or statistically significant differences found in disability and pain between combined strength training and stretching, and strength training alone.
- Muscle Strengthening - Strong muscles are a great support system for your spine and better handle pain. If core stability is totally regained and fully under control, strength and power can be trained. But only when this is necessary for the patients functioning/activities. This power needs to be avoided during the core stability exercises because of the combination of its two components: force and velocity. This combination forms a higher risk to gain back problems and back pain.
- Traditional Chinese Medicine for Low Back Pain - has been demonstrated to be effective. Reviews have demonstrated that Taping and cupping can be efficacious in pain and disability for chronic low back pain included disc herniation.
- Spinal Manipulative Therapy and Mobilization - Spinal manipulative therapy and mobilization leads to short-term pain relief when suffering from acute low back pain. When looking at chronic low back pain, manipulation has an effect similar to NSAID.
- Transcutaneous Electrical Nerve Stimulation (TENS) - TENS therapy contribute to pain relief and improvement of function and mobility of the lumbosacral spine.
- Manipulative Treatment - Manipulative treatment on lumbar disc herniation appears to be safe, effective, and it seems to be better than other therapies. However high-quality evidence is needed to be further investigated
- Traction - A recent study has shown that traction therapy has positive effects on pain, disability and SLR on patients with intervertebral disc herniation.Also one trial found some additional benefit from adding mechanical traction to medication and electrotherapy.
- Hot Therapies - may use heat to increase blood flow to the target area. Blood helps heal the area by delivering extra oxygen and nutrients. Blood also removes waste byproducts from muscle spasms.
- Cryotherapy - reduces spasm and inflammation in acute phase.
- Shortwave diathermy - pulsed SWD in acute condition and continuous SWD in chronic condition.
- Ultrasound - As phonophoresis, it increases extensibility of connective tissues.
The following program is an example of a protocol for rehabilitation following a lumbar microdiscectomy.
- Duration of rehabilitation program: 4 weeks
- Frequency: every day
- Duration of one session: approximately 60 minutes
- Treatment: dynamic lumbar stabilization exercises + home exercises
- Exercises: Prior to the DLS training session patients are provided with instruction or technique to ensure and protect a neutral spine position. During the first 15 minutes of each session stretching of back extensors, hip flexors, hamstrings and Achilles tendon should be performed.
- (DLS consists of: Quadratus exercises Abdominal strengthening Bridging with ball Straightening of external abdominal oblique muscle Lifting one leg in crawling position Lifting crossed arms and legs in crawling position Lunges)
- Home Exercises - should be added to the treatment. These should be performed every day. 5 repetitions during the first week up to 10-15 reps in the following weeks
Clinical Bottom line
- The initial treatment should be conservative, unless a patient has severe neurological compromise. Surgery is usually the last resort as it does not always result in predictable results. Patients are often left with residual pain and neurological deficits, which are often worse after surgery. Physical therapy is the key for most patients. The outcomes depend on many factors but those who particpate in regular exercise and maintain a healthy body weight have better outcomes than people who are sedentary.
- Intervertebral disc herniation is one of most common diseases that produces low back pain and/or leg pain in adults. It often occurs as a result of age-related degeneration of the annulus fibrosis. Disc herniation are most of the time asymptomatic and 75% of the intervertebral disc herniation recover spontaneously within 6 months.
- Disc herniation can occur at different levels in the spine. A herniated disc affects most commonly the lumbar discs between vertebra L4-L5 and L5-S1. Cervical disc herniation are more rare than lumbar disc degeneration. The cervical disc herniation is most locate at level C5-C6 and C6-C7.
Comments